You probably already know that a good night’s rest is vital to good health, but what if you just can’t sleep? If so, you’re not alone--experts estimate 1 in 3 people have at least mild insomnia. Lucky for you, this article will cover the most common causes of poor sleep and how you can remedy them.
The Signs and Symptoms of Perimenopause
Natural Solutions for Hormonal Symptoms with Dr. Mariza Snyder
Your Period After 40 with Dr. Lara Briden
Dr. Lara Briden is a naturopathic doctor and the period revolutionary—leading the change to better periods. Her book Period Repair Manual is out on its second edition with new sections on perimenopause, how to come off hormonal birth control and the different options for birth control. In this episode, we talk about the new book, perimenopause, managing heavy periods, and histamine intolerance.
Here's what you'll hear:
Min 02:10 Dr. Lara Briden's new book
Min 03:45 Feedback from Dr. Briden's first book
Min 04:30 What is perimenopause?
Min 05:55 The connection between hormones and symptoms of perimenopause
Min 11:10 Dr. Briden's rescue prescription for perimenopause moods:
Magnesium
Natural Progesterone
Taurine
Magnolia
Ziziphus
Ashwagandha
Vitamin B6
Min 20:20 Pregnancy in perimenopause women
Min 23:35 Managing heavy periods/flooding
Min 29:30 Going into perimenopause with health conditions
Min 35:35 Histamine intolerance
Min 44:15 Dr. Lara Briden's resources & help for teenagers
To learn more about Dr. Briden, visit her website here and follow her on social media:
Resources:
Period Repair Manual book
Perfect Periods Facebook Group
Hormone Balance After 40 summit
Prof Jerilynn Prior's article prescribing progesterone for heavy periods
Lara's article "The Curious Link Between Estrogen and Histamine Intolerance"
Here's a video version of the interview with Dr. Lara Briden:
Sign Up For Our Newsletter
If you have not yet joined our community, be sure to get our Hormone-Lovin’ Superfoods Guide here, and come on board!
We have lots of valuable, free resources for women's health we share weekly.
Get Your Brain Working Better with Dr. Steven Masley
Dr. Steven Masley, MD is a physician, nutritionist, trained-chef, and author. In this episode we talk about brain health and his new book "The Better Brain Solution" coming out Jan 2, 2018.
Here’s what you’ll hear:
Min 01:55 The fear of aging & brain health
Min 02:55 Introduction to Dr. Steven Masley
Min 03:25 Motivation behind the book "The Better Brain Solution"
Min 05:55 The 5 pillars to better brain health
Min 06:45 The odds of cognitive dysfunction for men & women
Min 08:35 Why women's brains rewire during menopause
Min 10:50 Other factors affecting brain health
Min 15:50 Exercise for improved brain health & insulin control
Min 19:30 Ketogenic diets, memory loss and interminent fasting
Min 22:10 Avoiding meat & grains when fasting
Min 25:00 Nutrients & supplements for a better brain
Min 30:10 Toxins (BPA, Phthaletes, Mercury), paleo eating & preservatives
Min 36:55 Dr. Steven Masley's brain quiz
To learn more about Dr. Masley, visit his website here and follow him on social media:
Facebook
Twitter
Resources:
Enroll for the 30-Day Better Brain Challenge
Sign Up For Our Newsletter
If you have not yet joined our community, be sure to get our free guide here, and come on board!
We have lots of valuable, free resources for women's health we share weekly!
Bridgit Danner, LAc, FDNP, is trained in functional health coaching and has worked with thousands of women over her career since 2004. She is the founder of Women’s Wellness Collaborative llc and HormoneDetoxShop.com.
Check out her easy 5-Day DIY Detox Guide here!
Using Chinese Medicine for Hormone Balance with Dr. Eric Karchmer
Dr. Eric Karchmer is a doctor of Chinese medicine and co-founder of DAO Labs. In this episode we talk about his clinical experience, the concept of Chinese medicine and how it applies to women's health, and Chinese formulas.
Here's what you'll hear:
Min 02:20 Introduction to Dr. Eric Karchmer & his education
Min 07:50 Dao Labs & Chinese medicine
Min 11:25 The concepts of Chinese medicine for women's cycles
Min 19:20 Eating cold food
Min 21:45 Blood deficiency & Dao Labs' formulas
Min 29:10 Formulas for perimenopause & menopause
Min 36:50 Selling formulas directly to consumers
Min 43:10 Formulas for PMS
Min 44:40 Seeing & treating clients
Min 47:35 Sourcing for herbs & testing for purity
Private Coaching with Bridgit
Check out our current coaching options on our website HERE.
Resources:
To learn more about Dr. Eric Karchmer & DAO Labs, visit their website here and find them on social media:
Facebook
Twitter
Instagram
Pinterest
Sign Up For Our Newsletter
If you have not yet joined our community, be sure to grab our hidden Hormone stressors quiz here, and come on board!
Thanks for listening,
Bridgit Danner,
Founder of Women's Wellness Collaborative
Why You're at Risk for Thyroid Disease After 40
Peri-menopause - the 5-10 years leading up to menopause - is a common time to be diagnosed with a thyroid condition.
In this article, I’d like to address these questions:
• Why then?
• Why more in women?
• What can be done?
Peri-menopause may begin in your late 30s or early or mid 40s. You may notice that your PMS is worse. You may have spotting between periods. Over time, your periods will likely get more dramatic, with missed periods and heavy periods.
Other symptoms may be popping up too, like anxiety, brain fog and weight gain. You may be thinking, “these sound like thyroid symptoms,” and you could be right!
But before we explore the thyroid connection, let’s cover what is normally happening during peri-menopause.
What is Peri-menopause?
Peri-menopause is, in short, the opposite of puberty. In puberty your ovaries are waking up to start your reproductive years. Your brain and ovaries are learning to work together to coordinate a monthly cycle, and often the first few reproductive years are hormonally unstable.
In peri-menopause, the brain-ovary relationship is starting to shut down. The ovaries are closing up shop, but the brain keeps knocking at the door, trying to get the shopkeeper working again.
The sex hormone that needs to rise sufficiently in the first half of the month is estrogen. It is produced by the ovaries as they also grow eggs. If you produce enough estrogen and release an egg, you’ll ovulate. And if that egg is healthy and hearty, you’ll produce a good amount of progesterone in the second half of your cycle. (The egg sac, or corpus luteum, makes progesterone after ovulation.)
How Your Thyroid Could Be Impacted in Peri-menopause
Even though both estrogen and progesterone are declining in peri-menopause, progesterone declines more dramatically in this stage. This leads to a condition called ‘estrogen dominance.’
Too much estrogen can prevent the thyroid hormone from getting to where it needs to go and can prevent it from converting to its active form. For some women, their thyroid symptoms are simply a result of this high estrogen interfering with thyroid hormone activity. We’ll talk about how to address estrogen dominance shortly.
Another thing estrogen effects is the immune system. Estrogen is associated with stimulating the TH2 branch of the immune system (1). TH2 is short for T Helper cell type 2, a lymphocyte (immune cell). TH2 is part of the adaptive immune system, which mounts a specific attack against pathogens.+ Adaptive immunity is usually a good thing, but it can also lead to autoimmunity if the antigen activity is directed towards itself.
As estrogen is the dominant sex hormone in women, this helps to explain why autoimmunity and thyroid disease is more common in women.
As we age, we also experience decreased immunity, and a tendency towards TH2 response.
“In the aged, however, naive cells are less likely to become effectors. In those that do, there is a documented shift towards a Th2 cytokine response.
The elderly have impaired ability to achieve immunization but much higher levels of circulating autoantibodies, (due to the lack of naive effectors) impaired response to viral infections, increased risk of bacterial infections, and increased risk of both neoplastic and autoimmune disease.” (3)
However, there is hope and action we can take to keep estrogen in check!
What To Do
1. Improve Gut Health
If you’ve studied the thyroid, you know that gut health is key to prevent an autoimmune response and to convert thyroid hormone effectively. Did you know it’s also important to clear estrogen dominance? One way your gut helps clear estrogen is through the estrobolome, “the aggregate of enteric bacterial genes whose products are capable of metabolizing estrogens.” (4)
You can be friendly to your gut by avoiding:
• Genetically modified foods (GMO) - These kill off friendly bacteria
• Sugars - These feed troublesome bacteria
• Unnecessary antibiotic use - This kills everything, with bacterial imbalance often resulting in its wake
You can be friendly to your gut by including:
• Small amounts of fermented foods like sauerkraut or kimchi
• A wide variety of fibers from salad greens, fresh spices, berries, etc.
• A long period from an early dinner to breakfast - lets your gut bacteria grow in peace!
2. Boost Progesterone
Progesterone helps keep estrogen in check, so boost it by giving your body ingredients to make hormones.
• Hemp Oil - I’ve been very impressed with how 1 T of hemp oil a day helps my own peri-menopausal hormones
• Borage Oil - This oil, usually in pill form, has gamma linoleic acid (GLA) to spark hormone production
• Maca- This adaptogenic root herb helps boosts hormone production and can benefit your energy levels and sex drive
3. Help Out Your Immune System
If aberrant immunity could be a problem in your case, add some components that can balance your TH2 activity:
• Omega 3 - Omega fatty acids have a balancing effect on the immune system and decreases inflammation. (5) Quality matters with omega 3, so do research to find a good brand.
• Vitamin D- Vitamin D deficiency is found at higher levels in people with autoimmune thyroid disease. (6) Talk to your doctor about getting your vitamin D tested and restoring it to a level around 60-80 NG/DL through sunshine and vitamin D3 supplementation.
Learn more about the thyroid at perimenopause from experts like Dana Trentini, Dr. Tom O’Bryan and Heather Dubé at the free, online Hormone Balance After 40 Summit!
The summit happens live June 5-11, 2017, but recordings will live on after the live summit.
Hormone Balance After 40 Summit
BUY the Hormone Balance After 40 Summit package here!
References:
1. http://www.ingentaconnect.com/content/ben/cdtia/2004/00000003/00000001/art00010
2. https://en.wikipedia.org/wiki/Adaptive_immune_system#T_lymphocytes
3. http://www.medscape.com/viewarticle/775536_2
4. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3264051/
Healthy Fats for Happy Hormones
In this article, we’ll be focusing on fats that increase the production of prostaglandins, which are not hormones, but are powerful, hormone-like agents that do important jobs such as regulating inflammation and stimulating hormone production. (1) So if you want to have regulated hormones and managed inflammation, read on to learn about your helpful prostaglandins and how to support them.
Are you dealing with symptoms like:
Hot flashes
Night sweats
Irregular periods
Heavy periods
Anxiety
Weight Gain
Menstrual migraines
These are all potential symptoms of inflammation and hormone imbalance that may benefit from the prostaglandin lovin’ you’ll learn about today.
What are Prostaglandins?
Prostaglandins are lipid compounds produced throughout the body, derived from fats and produced by an enzymatic process. They are made from Omega 3 and Omega 6 fats, plus some micronutrients and minerals are needed in their production as well.
Prostaglandins can both initiate and reduce inflammation. (2) Inflammation is a normal process in the body, but too much inflammation causes pain and hormone dysregulation.
Since prostaglandins can be inflammatory or anti-inflammatory; one way to reduce symptoms is to increase anti-inflammatory prostaglandins by consuming the fats that are needed to make anti-inflammatory prostaglandins.
If you’re nutritionally savvy, you may have learned that Omega 3 fats are good and that Omega 6 fats are bad. This is somewhat true, but there’s more to it.
The Fats
Omega 3 and 6 fats are both polyunsaturated fatty acids, and the numbers 3 and 6 refer to the location of a double carbon bond within the structure of the molecule. Omega 3 and 6 oils are considered ‘essential’ to consume because the human body cannot make them.
The Omega 3s
Omega 3 oils are anti-inflammatory which means they reduce the unwanted symptoms of inflammation like headaches and acne. Their anti-inflammatory effect even helps in treating the autoimmune diseases that are becoming so common in women by regulating the immune system.
The three types of Omega 3 fatty acids involved in human physiology are α-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA). ALA comes from plant sources and DHA and EPA come from marine sources.
ALA sources of omega three can be converted in EPA and, less efficiently, to DHA. There has been some debate about the rate of this conversion. It appears that women, as a result of higher estrogen levels, convert ALA to EPA at a higher rate than in men. (3)
EPA is what we are focusing on in this article, as it is converted to a prostaglandin.
From the Omega 3 category, consume foods such as:
Wild, fresh salmon
Grass-fed beef and lamb
Pastured chicken or duck eggs
Fish eggs
Sardines
Tuna
Oysters
Shrimp
Anchovies
Flounder
Bass
Mackerel
These vegetarian sources of Omega 3s are awesome additions to your diet:
Fresh ground flax seed
High lignan flax oil (use for dressing, not for cooking)
Walnuts
Chia seeds
Leafy green vegetables like spinach and kale
Brussels sprouts
Sea vegetables
Hemp seed and oil
As a supplement, you can take 1,000 mg /day of high quality fish oil, like this one we carry. You can also find an algae-based Omega 3 oil as well, like this one from Nordic Naturals.
The Omega 6s
While all clean sources of Omega 3's are good, Omega 6's are more of a mixed bag.
Omega 6 oils include linoleic acid (LA), an essential fatty acid, and gamma-linolenic acid (GLA). Similar to the conversion process of the Omega 3 ALA into EPA, it is possible to CONVERT LA into GLA, but there can be snags in the process. Another downside of linoleum acid is that too much is inflammatory.
So it’s best to get your linoleum acid from clean sources, and also to add in the lesser-known and potent GLA oils below.
The Bad Boys
Some Omega 6 fats are dangerous, like the ones coming from canola, corn, safflower oils. These processed vegetable oils often are derived from non-organic, genetically-modified seeds, and the oil can only be extracted from a series of complex steps. In other words, they are not real food. The resulting product is inflammatory, can contribute to leaky gut, and can actually block normal hormone production and function, contributing to things like cramps and infertility. (4)
These oils are prevalent in processed foods like bakery items, margarines and most prepared foods, whether from the grocery store shelf, the deli section or a restaurant. When you use these oils to fry things like French fries, they become really bad, as the extra heat exposure creates even more free radicals.
Please do not use vegetable oils in your home cooking and avoid all margarines. Minimize processed foods and cook at home much more than you eat out.
The Good Girls
Clean sources of linoleic acid (LA) include:
Avocado
Almonds
Brazils nuts
Pistachios
Pecans
Pine nuts
Sunflower seeds
Organic organ meat
Great sources of gamma- linoleic acid (GLA) include:
Borage oil
Evening primrose oil
Flax oil
Olive oil
Hemp oil
Spirulina (5)
As mentioned earlier, LA can be converted to prostaglandins, but too much compared to Omega 3 ALA can be a problem. (6) So watch your ‘bad boy’ oil consumption. And do get your extra special GLA fats, as these are not inflammatory and tend to be the most overlooked in our diets.
It can be easy to increase good fats in your diet. Here are some suggestions:
Drizzle hemp, flax or sesame oil over your cooked food or salad.
Buy raw nuts and mix with coconut flakes and dried berries for a trail mix/ easy snack. (Store in fridge.)
Add nuts and seeds to your morning smoothie.
Make a chia/ seed porridge.
Find a clean source of fish and learn to cook it!
Learn about sea vegetables and how to use them.
References:
Before the Change: Taking Charge of Your Perimenopause by Ann Louise Gittleman, Harper Collins 1998
http://www.marksdailyapple.com/why-the-omega-3omega-6-ratio-may-not-matter-after-all/
Bridgit Danner, LAc, FDNP
Founder of Women's Wellness Collaborative
Bridgit Danner, LAc, FDNP, is trained in functional health coaching and has worked with thousands of women over her career since 2004. She is the founder of Women’s Wellness Collaborative llc and HormoneDetoxShop.com.
Support These Three Systems for Smoother Peri-menopause
We'll focus on three systems to support the most while in peri-menopause.
1. Balance Your Blood Sugar
This tip is HUGE for peri-menopause, so pay close attention. When you were younger, you could maybe get away with late-night pizza or drinking binges. You body is much less forgiving at this age, which you probably already realized.
You don’t want to gain weight, feel cloudy, or sleep poorly, but, if your like most of us, you want to have you cake and eat it too.
It’s super important to keep your blood sugar balanced to prevent the symptoms of peri-menopause. Spikes and dips in your blood sugar create an additional stress on your body, and your body is already going through the stress of changing hormones.
These spikes and dips in your blood sugar also make you cranky, craving carbs and gaining weight. Sugars also feed the unhealthy bacteria in your gut, and you need a healthy gut to clear old hormones and to make chemicals that make you feel good.
Here’s my best tip for blood sugar: start the day with low sugar and high protein and fiber. When you start you day this way, you will have less cravings and make better choices.
Some options:
Eggs
Trail mix
Leftovers from dinner
Organic breakfast sausage
Miso soup with veggies
2. Love Your Adrenals
Your adrenals are two glands in your lower back that make hormones for energy and stress. They also make some female hormones (sex hormones) and you rely on them more as your ovarian function declines.
Your adrenals make hormones for stress, energy and sex. You probably want lots of energy and great sex, but less stress. So create less stress in your life.
Now, you probably think of stress as being stuck in traffic and late for an important appointment. That is stressful. But stress to your body comes in lots of other forms too, like:
The blood sugar spikes and dips we discussed
The late nights of work
The stress of caring for kids or elderly parents
Chronic pain
Eating low-quality foods or inflammatory foods
This list could be longer, but I’ll stop here and give you tip #2 to love your adrenals. Get to bed by 10 PM, take rest breaks during the day, and have fun!
3. Support Detox Pathways
To have hormone balance, you need to clear toxins. Excess hormones re-circulating in your blood stream, or toxins that mimic hormones can lead to peri-menopause symptoms.
Today we’ll talk about two mechanisms that clear toxins and how to support them: the liver and the digestive tract.
The liver is the best known detox organ, for good reason. It breaks down toxins and used hormones into a form that can be eliminated. To support the liver, eat foods that contain the nutrients your liver needs to do its tasks.
Some liver-loving foods include: pasture-raised eggs, beets, carrots, lemon, broccoli, chard, dandelion, cabbage, onions and garlic.
Once toxins and used hormones are broken down, they need to be eliminated from the body. The main exit route is the digestive tract. If you are constipated or have an inflamed digestive tract, these waste products may not be eliminated.
Natural sources of fat, such as coconut oil, olive oil, nuts, seeds, avocados, unprocessed meats and fish, are needed by the gallbladder to make the bile that the toxins travel with from the liver to the digestive tract.
Once in the digestive tract, keep your bowels moving with regular exercise and drinking plenty of water. Reduce inflammation by avoiding inflammatory foods such as sugar, alcohol, gluten and processed dairy products.
Please take one tip from above and get started!
Love these tips? Want to learn more?
Learn more about peri-menopause from experts like Ann Louise Gittleman, Dr. Anna Cabeca and Tana Amen at my online Hormone Balance After 40 Summit!
The summit happened live June 5-11, 2017, but recordings will live on after the live summit.
You’ll hear 30+ experts on the topics like:
• Boosting your Metabolism
• Reclaiming your Sex Drive
• Restoring Mental Clarity.
The best part is that it’s all free and you can attend online from any computer or smartphone. Purchase here for your own Hormone Balance After 40!
What in the World is Peri-menopause?
If I were to ask 10 women on the street, “What is peri-menopause?,” I would probably get just 1 out of 10 who would know the answer, at best.
Peri-menopause is the about 10 year period before the full stopping of your period, called menopause. The stopping of your menstrual period doesn’t just come out of nowhere, it happens after a slow decline of ovarian function.
Your ovaries, the two little organs that shoot out an egg every month when you ovulate, come to life at puberty, and peak around 27 years of age. After that, their function starts to decline very gradually, and then much more rapidly.
If you recall your teenage years, you may remember having acne, mood swings and irregular periods. This was because your brain was learning to work with your newly active ovaries together.
At peri-menopause, you may also have hormonal symptoms, that could include:
Heavy periods
Early periods
Missed periods
Anxiety
Insomnia
Weight Gain
Forgetfulness
So why do the symptoms of peri-menopause happen?
Sadly, you can’t live forever, or make babies forever. Your genes are programmed to turn on your reproductive powers at puberty, and gradually fade them before menopause.
As you entered puberty, your ovaries started making estrogen, the dominant female hormone, like crazy. You grew breasts and hips and your periods may have been really intense.
You rode this nice estrogen high with gorgeous skin and a healthy sex drive in your 20s. But as you aged, your ovarian function declined and you made less estrogen, slowly.
Just like in puberty, the brain is trying its best to work with the ovaries at peri-menopause. Some months it's pushing them to work harder, and estrogen level go up. Other months estrogen levels are low. This is a normal aspect of peri-menopause, but it can result in symptoms.
Because the eggs in the ovaries aren't as prime in our older years, their function is less robust. This leads to less progesterone production, the hormone that is made after your ovulate, in the second half of your cycle. It is also normal that progesterone declines, but this change can again cause symptoms.
Here’s one last detail: you make a certain type of estrogen, estradiol, in your reproductive years. As you shift towards menopause, another type of estrogen, estrone, becomes dominant. But that shift is a little rough on your body, because it got used to using estradiol for many years.
You don’t have to be a victim of your changing hormones. Once you get to know your hormones and what they need, you can be the hero in your own hormone story.
Stayed tuned for information on how to best take care of yourself in these years to avoid symptoms as much as possible!
Bridgit Danner is at the author of this article and the founder of Women's Wellness Collaborative.
She designed a private, collaborative coaching service exclusively for women which utilizes the accuracy of functional medicine for outstanding results.
What to Do About Heavy Periods
Are you avoiding social events because of your heavy period? Missing work? Soaking through a great outfit, or your mattress? How about getting on birth control for your wedding to avoid a blood bath on your special day?
If you have heavy periods, they can be very inconvenient. They can also be exhausting.
I always say that your period blood isn’t ‘extra blood’, it’s real substance that your body made with work and nutrients. And it’s work to make it all over again. Now, if you health is good and your flow is normal, it’s all good. But when your flow is excessive, you can end up depleted.
This article will help define what a heavy period is, why it happens, and some great ideas on what to do about it. So let’s get started!
1. How Much is Too Much Menstrual Bleeding?
The range of normal flow is 10-60 ml, according to the National Health Service of the UK.
According the Centre for Menstrual Cycle and Ovulation Research, the average flow a woman has is 30 ml, or 2 Tablespoons. It doesn’t sound like much, but it’s 6 soaked tampons or pads. Considering that most women will have a heavy day or two, and a few light days (4-6 days in total), this sounds about right.
Over 60 ml or over 80 ml (depending who you ask), i.e. 16 soaked menstrual pads, is considered menorrhagia- very heavy menstrual bleeding often with clots and flooding. Women in last category will often experience iron-deficient anemia (inadequate red blood cell count).
While it’s normal to have a heavy day or two, if you have to always pair a tampon with a pad, or re-arrange your schedule around your flow, it’s too much. If you have heavy multiple heavy days, like 4+ heavy days, it’s also too much. If you find yourself very exhausted and short of breath due to your period, these are further symptoms.
2. What Causes Excess Menstrual Bleeding?
The most common reason for heavy bleeding is estrogen dominance. First let’s define estrogen, and how it affects your cycle.
Estrogen is a hormone that influences many processes in your body, from bone formation to clear thinking. Estrogen is mainly made in the ovaries, although it can also be made by the adrenal glands or in your fat tissue.
Each time you have a period, your hormone levels drop. When they drop, the brain registers this change and signals your ovaries to make more estrogen. This estrogen ripens a new egg for the next period cycle, and the estrogen grows your uterine lining.
This growth phase is fairly short. You have your period for 4-6 days (ideally), and then your build the lining up for about another ten days. At day 14 (ideally), you ovulate. While you continue to make estrogen, another hormone, progesterone, becomes the dominant player after ovulation. The progesterone firms up and matures your uterine lining, making it hospitable for a potential pregnancy.
Now let’s say this ideal picture is disturbed by too much estrogen, or not enough progesterone to balance out the estrogen. Then you get more growth in you uterine lining. This means more blood at period time, and can lead to big clots too.
There are lots of reasons for estrogen dominance. Not all of them will apply to you (: So I’m giving a clear heading for each type, so you can scan over them and see which may be a match for you. In section three, we’ll cover ways to address these issues, so keep reading!
A. You Are Getting Your First Periods
When you have your first period as a young woman, estrogen levels pump up! As your ovaries come to life, your brain and ovaries learn how to dance together, and your first few years of cycling can be irregular. Heavy, painful periods are commonly reported in teenage women.
This does not mean you have to just accept your fate or get on birth control pills. Many young women have a poor diet and are being exposed to chemicals and growth hormones. Please see the ‘What Can You Do About Heavy Bleeding?’ section for tips!
B. You are Overweight
Your fat cells house an enzyme called aromatase, used in the manufacture of estrogen. The higher your percentage of body fat, the more estrogen you can produce. As you reduce stored body fat, your estrogen production will lessen as well. Ironically, when you lose weight you will release estrogen that was stored in that fat tissue, and you can become more hormonally imbalanced in the process. So lose weight at a moderate pace.
As you age, the lowered amount of estrogen you produce can slow your metabolism and lead to more weight gain, especially in the middle. Conversely, the amount of estrogen you produce in your fat and other peripheral locations can cause an estrogen overload and heavy periods. Sometimes it’s just not fair! (Source)
C. You are Exposing Yourself to Chemicals and Food Additives
Before I became educated, I would look at my shampoo bottle and its list of chemical ingredients and think, “well I’m sure these are safe for me or they wouldn’t be in here.” Nope.
According to a 2013 article in the NY Times, “In its history, the E.P.A. has mandated safety testing for only a small percentage of the 85,000 industrial chemicals available for use today. And once chemicals are in use, the burden on the E.P.A. is so high that it has succeeded in banning or restricting only five substances, and often only in specific applications: polychlorinated biphenyls, dioxin, hexavalent chromium, asbestos and chlorofluorocarbons.”
Many of these chemicals are xenoestrogens, or chemical compounds that look like estrogen to the body. When these chemicals get inside of you, through eating them, rubbing them on your skin, or inhaling them, they attach to estrogen receptors in the body. That means your cells get the estrogen message, and to the uterine lining that means “grow”!
That’s why it’s so important to limit your exposure to these compounds, at any age. For a some women, these compounds could mean heavy periods. For other women, they can contribute to breast and other cancers. (Source)
D. You Have an Underactive Thyroid
Thyroid disease is skyrocketing in our culture. According to the American Thyroid Association, more than 12 percent of the U.S. population will develop a thyroid condition during their lifetime and women are five to eight times more likely than men to have thyroid problems.
Your low thyroid activity can lead to low reproductive hormone production. This can mean you don’t ovulate as often, or that you make less progesterone.
When you have low thyroid activity you also have decreased sex hormone binding globulin (SHBG), which can mean that more estrogen in circulation, leading to heavy periods. (Source)
To complicate matters, high estrogen can bind up thyroid hormone, feeding the imbalance!
E. You Are Not Ovulating
Here’s some news that most women don’t seem to know; just because you have periods doesn’t necessarily mean you are ovulating. Sometimes the body seems to be cycling, because it is trying to achieve that, but it’s kind of going through the motions.
This can be due to stress, due to being underweight or nutrient deficient, due to perimenopause, or due to polycystic ovarian syndrome (PCOS). Whatever the cause, if you don’t ovulate, then you’re going to make less progesterone (which is made after ovulation), so you won’t have that to balance out the estrogen production.
If you don’t ovulate you can also get your period in a very delayed timeline, so then the estrogen is left unchecked for even longer.
F. You Have Low Progesterone
This cause is a cousin to the ‘you are not ovulating’ cause above. Even if you do ovulate, if you ovulate a poor quality egg, or have other hormone production problems, then the estrogen is left somewhat unchecked. This may also cause spotting and breakthrough bleeding in weeks 3-4 of your cycle.
G. You Are in Perimenopause
During perimenopause (the ~ 10 years before menopause), you ovarian function starts to decline. The eggs are generally not as good of quality anymore, though some are better than others. Estrogen is being made well some months, and not so well other months. So some months you’ll have a more normal cycle, and other months you can flow quite early, late or heavily.
To some extent this is ‘normal’, as the body is aging and getting ready to leave its reproductive phase. (It’s sad; I know.) But there are ways to ease the transition too.
H. You Have Fibroids or Endometriosis
Fibroids are masses that form in or on your uterus. Estrogen dominance is generally to blame for how these grow in the first place. Then to make matters worse, they respond to the cyclic hormonal changes of your menstrual cycle, and grow and shed like your uterine lining.
This can cause very heavy bleeding and can lead to anemia.
Some women can have a separate condition called endometriosis. Uterine tissue migrates outside the uterus, for example, around the abdomen. When a woman menstruates, endometrial tissue - wherever it is in the body - bleeds.
I. You Have Recently Given Birth or Had a Miscarriage
Birth
After I gave birth to my son, I was shocked by how much bleeding I had for so long. Though everyone generously gave me blankets and baby toys, no one warned me about this!
According to the folks at What To Expect, “the heaviest of the bleeding will last for about three to ten days after labor and delivery and then it should taper off to lighter spotting after pregnancy. You'll see the difference in the color as this starts to happen, from red to pink, then brown, and finally to a yellowish white. Lochia (mix of blood, mucous, tissue) should stop flowing around four to six weeks after delivery.”
I definitely remember bleeding for a least a month. If you continue the bleed heavily after 10 days (like changing a pad every hour), contact your doctor. Even if you had a C-Section, you will still be expelling blood and loch after birth.
Miscarriage
I have never had a miscarriage, but I’ve heard some horror stories from my clients.
If you are less than eight weeks pregnant when the miscarriage occurs, the expelled tissue will look no different from heavy menstrual bleeding. The further along you are in pregnancy, the heavier the bleeding and more severe the cramps.
According to Maricopa OBGYN page,
“During the miscarriage, you may bleed heavily, soaking a pad every 10 minutes. The cramping can be quite uncomfortable.
Although cramping, bleeding and occasional clotting is normal after both a miscarriage and a D&C, you should not be soaking more than 2 pads an hour nor experience worsening, exquisite pain after the uterus has been emptied. These are important symptoms to report to you doctor.
During your recovery, you will continue to bleed, on and off, for up to 3 weeks. Some minor cramping will continue in the next few days also. If bleeding increases or stays bright red, or if you have foul-smelling discharge or a fever or persistent cramping, contact your health care provider.”
J. Uterine and Cervical Cancer
It is possible that heavy bleeding could arise from uterine or cervical cancer. These conditions could involve heavy flow or spotting at random times, or after sex. The odds are that your heavy flow or spotting is due to an item in above list.
Cervical cancer usually will not process to heavy bleeding unless the disease is quite progressed. The best prevention is to practice safe safe and to get a pap smear every 5 years or as directed by your physician. Cervical cancer often develops from certain strains of the Human Papillomavirus (HPV).
Uterine cancer is more comely diagnosed in women over 50 years old, although there are other risk factors such as obesity and a history of irregular cycles. Every year, about 52,000 U.S. women are diagnosed with uterine cancer, according to the National Cancer Institute.
K. Hemophilia
It is possible that you will have heavy bleeding due to a blood clotting disorder. If you are missing clotting factors VIII or IX, you will also experience easy bruising or nose bleeds, and can have very heavy bleeding after childbirth. You will probably have menstrual pain as well. This condition is rare, 1 in 5,000 - 10,000 for type A and 1 in 50,000 - 100,000 in type B, but if you suspect this, especially if there is heavy bleeding in your family, ask your doctor.
3. What Can You Do About Heavy Bleeding?
As I shared above, the most common reason for heavy bleeding is estrogen dominance, so let’s start there for solutions:
A. Avoid Xenoestrogens
Xenoestrogens are synthetic chemicals that look and act like estrogen in your body. When these are present, it’s easy to get into estrogen dominance and heavy periods. The top tips are:
Eat organic
Use all natural cleaning and beauty products
Avoid using plastics for cooking and food storage.
B. Watch your Weight
Estrogens are also made in your fat tissue through a process called aromatization. If you are trying to eat right and exercise but can’t lose weight, avoid xeno-estrogens, check your thyroid, make sure you get a good night’s sleep.
C. Check Your Thyroid
I love Izabella Wentz’s ‘safety theory’ that theorizes that when your body is under stress (emotional, chemical, or pathogenic), it dials down thyroid production as a way to get you to safely hibernate. It’s fascinating. Read about it here.
If you do get your thyroid checked, be sure to do it up right, getting a full thyroid panel and having it interpreted by a functional medicine type practitioner. Jen Wittman of Thyroid Loving Care has some great info on that here.
D. Try Herbs and Supplements
I am not a fan of using supplements unless you have a solid base of good habits, and have checked for other underlying causes. But I will mention a few nice supplements here, and you can check with you doctor if it’s safe for you to use them.
1. Vitex - This herb, that is also called chaste tree berry, seems to benefit communication between your ovaries and your brain, and it’s especially good at increasing progesterone. It may not be as useful for women in their late 40s, and it may not be a fit for everyone, but it has many success stories. It can be taken daily throughout your cycle. Use for 6 months, unless you have an adverse reaction.
2. Di-Indoly Methane (DIM)- DIM is a star at clearing excess estrogen. It’s often used for PCOS (polycystic ovarian syndrome) but it can be useful in most any case of estrogen dominance. For more information, see this blog at NaturoDoc. According to Dr. Holly Lucille, ND, RN, DIM shifts estrogen metabolism to the healthy 2-hydroxy pathway (makes for nice skin) in place of the troublesome 16-hydroxy pathway (makes for heavy periods and cancers).
3. Calcium-D-Glucarate (CDG)-This is one I’ve just learned about recently. CDG also does a great job at clearing spent estrogen from the body. Here’s some cool information on how it works from Dave Asprey at bulletproof.com:
“One of the ways the body gets rid of toxins is through a process called conjugation. During conjugation, toxins are packaged into water soluble compounds called glucuronides. Glucuronides are meant to pass from the liver, to the bile, then to the gut where they are excreted. However, high levels of an enzyme called beta-glucuronide can inhibit this process. This enzyme separates toxins from their conjugate bond and allows them to be reabsorbed. This allows toxins to keep circulating in the body where they make you fat, tired, and weak.
Calcium-d-glucarate prevents beta-glucuronide from disturbing this process. It keeps the toxins bound inside a glucuronide which is then removed from the body. Toxins are most damaging in their free form, which is why you want them to be bound (conjugated) and released from the body. Calcium-d-glucarate inhibits beta-glucuronidase which allows toxins to be removed.”
E. Heal Your Gut
You might be surprised to hear that your digestive tract has anything to do with heavy periods! But it’s so. Your gut is the place where food is broken down into the nutrients you need to make hormones. It’s also the place where used hormones are broken down and expelled. So it needs to be a healthy environment, free of inflammation, full of good bacteria, and moving daily.
This is a big topic to cover, but here are two top tips:
Chew your food and eat a relaxed fashion. Gulping down food while scanning your smartphone does not lead to proper digestion.
Eat a variety of fibers daily/ weekly. Fibers from berries, nuts, seeds and vegetables will fuel the friendly bacteria in your gut. And don’t get stuck eating the same 4-5 things; mix it up for greater bacteria diversity.
F. Try Chinese Medicine
Chinese medicine can be a relaxing way to balance your hormones. Herbal formulas like Bu Zhong Yi Qi Tang, and treatments like moxibustion on your spleen 1 point can stop a heavy flow. Look for a practitioner who specializes in women’s health in your area. If you’re in Portland, Oregon, come check us out at Blue Sky Wellness Studio.
G. Zen Out
A major hormone disruptor is stress. It blocks hormone receptors, raises blood sugar and blocks production of reproductive hormones. The reproductive hormone that goes down first is usually progesterone, and you’ve learned you need that to balance out the estrogen.
My best advice here is to focus on having fun. If you stay connected with friends, go to a delicious meal with your sweetie, or take a work break to visit the sauna (I did this today), it’s hard to stay obsessed with your problems. Problems will always be there, so seize the moment and enjoy life!
H. Seed Cycling
Seed cycling means taking certain nuts and seeds in the first 2 weeks or your cycle, and another type in the second two weeks. The alternating phases support first your estrogen production and then your progesterone production, plus the fiber helps clear spent hormones. I already wrote a whole blog on this topic, which you can access here.
Wow, thanks for sticking with me and reading this very long article on heavy periods! I hope it helps you. If you’d like more in-depth support, we offer private health coaching here.
Bridgit Danner, LAc, FDNP
Founder of Women’s Wellness Collaborative
Is Low Progesterone Behind Every Hormone Problem?
This article is suitable for: Perfect Periods, Fertility, Post-Partum and Perimenopause
Wondering what the heck is happening with your hormones?!?
I am creating a new online quiz, and as I compiled the reasons behind various conditions- PMS, infertility, postpartum depression, disruptive menopause- one reason was dominating the answer field: low progesterone.
I don’t know why the sheer dominance of the pattern just hit me now after years of research! Hopefully I can save YOU a few more years of hormonal confusion with this article. This article is suitable for women in any stage of life!
What is Progesterone?
Progesterone is a hormone made primarily in the ovaries by the corpus luteum (the tissue left behind after you release an egg at ovulation). It is also made by the adrenal glands, and if you are peri-menopausal or menopausal with infrequent or no ovulation, then you really rely on the adrenals as a source of progesterone.
Progesterone has various functions in the body:
After your ovulate, it helps ‘ripen’ your uterine lining, preparing for a possible pregnancy
Raises your basal body temperature in the second half of the cycle
Serves a precursor hormone to cortisol, your energy/stress hormone made by the adrenal glands
Lifts you mood and calms your body
Benefits sleep
Prevents water retention
Helps the cells utilize fats
Helps maintain blood sugar levels
You can surmise by the list above that if you are low in progesterone, you may have some of the opposite effects- bloated, moody, can’t sleep, craving sugar, gaining weight, and periods are irregular or heavy.
How Does Low Progesterone Happen?
Low progesterone can occur for many reasons that are very common in modern life, which is likely why I am seeing this pattern so frequently with my clients.
1. Estrogen Dominance
Estrogen dominance is both a cause and a result of low progesterone.
It’s a cause because you can get too high in estrogen due to carrying excess body weight, and your fat tissue produces estrogen. Even if you are thin, you can put yourself into excess estrogen if you have high blood sugar and insulin resistance. Insulin resistance is a state in which your cells block insulin from getting inside because your blood sugar is too frequently too high.
Symptoms of blood sugar dys-regulation include: feeling hungry all the time, getting very irritable if you miss a meal (or a snack), fatigue, weight gain around the middle, acne.
The most common hormonal disorder amongst women of reproductive age is PCOS, or polycystic ovarian syndrome. In this condition, there is insulin resistance, high androgen production, and disordered function of the ovaries. This often leads to missing or infrequent ovulation. As you learned already, most of our progesterone is made after you ovulate, so you don't ovulate, then you won't make much progesterone, and you'll be in estrogen dominance.
Another major disruptor are xenoestrogens, which are synthetic compounds that activate estrogen receptors in the body.
Some key sources of xenoestrogens are:
Commercially-raised meat and dairy products
Medications, including birth control pills
Non-organic foods (with traces of pesticide)
Soft plastics
Shampoos, body lotions and perfumes (contain xenoestogenic compounds unless all natural)
Tap water
Food additives
Bleached tampons and sanitary pads
You can see that it’s easy to get exposed to a lot of xenoestrogens in day! The xenoestrogens in your body confuse the feedback loop between your brain and your ovaries. If your liver is overloaded, you won’t break down these xenoestrogens well, and they can get stored up in fat tissue (hello, belly fat) for you body to handle later.
Here’s an article by the Environmental Working Group if you’d like to deepen your research on this topic.
Even if you don't have excess estrogen, if progesterone is low, you can still end up in estrogen dominance.
Estrogen and progesterone play a seesaw game over the course of a month, and over the course of your life as a woman. Estrogen is needed to stimulate your ovaries and grow your uterine lining in the first part of your cycle. This strong first half leads to strong progesterone in the second half, unless something goes wrong. The following points can all be causes of low progesterone.
2. Poor Nutrition
With the busyness of modern life, it’s easy to choose processed foods, caffeinated drinks and sugary pick-me-ups. Living in a grind, without time to reflect and connect, can also draw us towards ‘comfort food,’ or that after-work glass of wine.
Besides these easy-to-make poor choices of modern life, even organic food is not as nutritious as it used to be, due to decreased soil quality. And let’s face it, we don’t alway eat organic, whether it’s because we don't have access, we can’t afford it or we’re eating out.
The last point I’ll mention here is weak digestion. When we’re stressed, have taken antibiotics, don’t chew our food, etc., we aren’t getting the most out of the food we eat.
How does this contribute to low progesterone? We need certain ingredients to make and utilize hormones. You need enough B6 and cholesterol for progesterone production, but there is more to it than that. All our micronutrients (vitamins and minerals) and macronutrients (protein, fat and carbohydrates) are needed for the proper functioning of our coordinated hormonal system.
3. Stress
You are a highly productive woman, but you are likely under chronic stress. (If not, congratulations!) Stress can come from so many places: your commute, the chemicals in your environment, a tense relationship, an undiagnosed dental infection, etc. Chronic stress makes your adrenal glands react with a high level of cortisol…at least at first. In this stage you may feel wired, not be able to sleep, not be able to focus on sex, feel anxious, etc.
As you learned earlier, progesterone is a precursor to cortisol. So if you are making lots of cortisol, is it fair to assume that your progesterone level is being affected? Yup.
Image courtsey of Functional Diagnostic Nutrition (TM)
Have a look at the chart to the right. Not only will you burn through progesterone to make cortisol, your body will start to favor that pathway at the expense of your other sex hormones: testosterone and estrogen (pictured at lower right).
Remember how you learned earlier that progesterone is made mainly by the corpus luteum? There is another hormone that is needed to get you to a nice, strong ovulation: estrogen. Estrogen is made by the ovaries, upon signaling by your brain, to stimulate your ovarian follicles and mature a healthy egg in the first half of your menstrual cycle.
This is why we can’t overly focus on the low progesterone aspect. We have to look ‘upstream’ at what other hormones are being affected and what’s really behind our imbalances.
Low cortisol can be related to some other symptoms like catching colds and flus frequently, getting dizzy easily, or feeling overwhelmed easily.
4. Perimenopause
Perimenopause is the ten year period before menopause during which your ovarian function is declining. For some women, they are still getting a period pretty regularly and feeling pretty good. For others, this ten year period can be tumultuous. After learning about stress and nutrition above, I’m sure you could guess these things could play in to a rockier perimenopause.
But this declining ovarian function is natural. As your egg quality declines with age (even if you’re enjoying low stress and good nutrition) you could still fail to ovulate, or ovulate a ‘weak’ egg, and its corpus luteum may not produce as much progesterone.
As you learned earlier, the adrenals can pick up some slack…as long as they aren’t depleted from years of stress and malnutrition!
There is another change that is occurring too, especially as you get close to menopause: the main type of estrogen you use is changing form estradiol to estrone, and this a big switch for your body. You have different receptors for estradiol versus for estrone, so there can be some ‘wobbles,’ such as memory lapses or hot flashes as you go through this process. You can also have what feels like constant PMS, and that’s no good! Be sure to read our ‘what to do to support progesterone’ section at the end of this article.
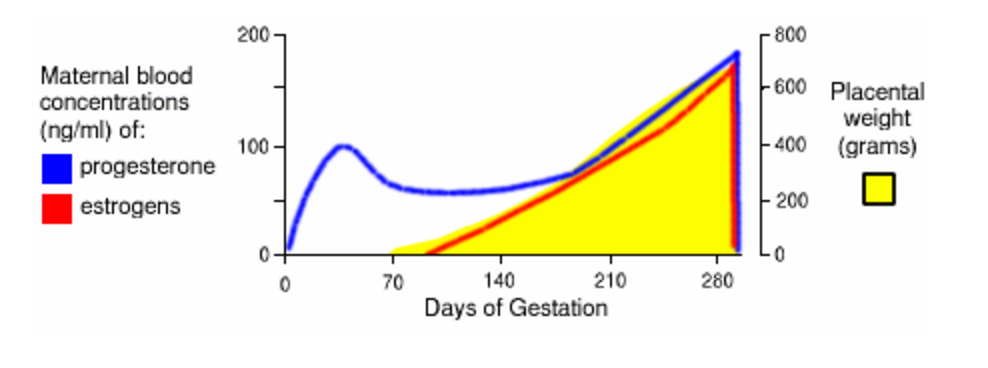
5. Postpartum
What’s another time that you are not ovulating for natural reasons? Pregnancy and postpartum! While you are pregnant you are on a hormonal high, with corpus luteum and then the placenta producing producing very high amounts of estrogen and progesterone, up to 30-50 times higher than your non-pregnant level!
But after childbirth, your hormones levels drop like a bad habit. This can produce some of the same reactions as in perimenopause, like night sweats and depression.
As you breastfeed, you are high in the hormone prolactin, and that inhibits ovulation. As you are learning no ovulation leads to low progesterone. Again, your adrenal glands can pick up the slack, but if you came into pregnancy with moodiness and poor stress-handling, you likely will end up there again after childbirth. Be sure to read through for our 'fixes' at the end!
6. Low Thyroid Function
Lastly, let’s learn about low thyroid function. If you have an under-functioning thyroid, whether due to Hashimoto’s thyroiditis or another reason, it can affect your progesterone. This happens in two ways:
When you have low thyroid function, you have decreased sex-hormone binding globulin (that’s a mouthful) which binds up sex hormones like estrogen, possibly letting estrogen levels get too high compared to progesterone.
Because thyroid hormone stimulates activity in every area of the body, when thyroid hormone is low, your production of sex hormones will be low.
It’s estimated that up to 15% of Americans have thyroid disease, if you include subclinical hyptothyroidism. Up to 10% of women will experience post-partum thyroiditis. Women are 5-10% more likely to have thyroid disease than men, and the age group over 50 is most at risk. (Source: Your Healthy Pregnancy with Thyroid Disease by Dana Trentini and Mary Shomon,.
How are we getting to this heightened incidence of hypothyroidism? Again, the factors of modern life are the perfect storm for it: high stress, toxins everywhere, an ‘altered’ food supply.
Autoimmune Hashimoto’s Thyroiditis is the leading cause of hypothyroidism. The gut, as we discussed in the Poor Nutrition section and will discuss again in the closing section, is a key area of focus in healing Hashimoto’s. When peptides (parts of the protein in foods) cross the gut barrier into the blood stream it stresses the system and the immune system responds by going after those peptides that shouldn’t be there. But the trouble is that this dysregulated immune system will also attack the body’s own tissue, in this case the thyroid gland.
The most touted symptoms of low thyroid are foggy thinking, cold limbs, fatigue, hair loss, constipation and weight gain. But I fight with hypothyroidism and I am skinny and tend more towards loose stool, and luckily still have all my hair! There are many manifestations of hypothyroidism, so it’s worth taking a deeper look if you suspect you may have hypothyroidism. A great place to start looking is the website of Dr. Izabella Wentz, aka the Thyroid Pharmacist.
What to Do to Support Progesterone Production:
Herbs and Supplements:
Maca- Maca is an adaptogenic herb, meaning it can adapt to find and serve the needs of your body. It can increase your energy by supporting your adrenal glands. My friend Dr. Anna Cabeca, who developed a green drink mix called Mighty Maca, says that in a before and after lab test, her client’s DHEA doubled using Might Maca. DHEA is a precursor to our sex hormones estrogen and testosterone, so that’s great news! Testosterone, by the way, is the dominant sex hormone in men, but women do need and want it for sex drive, muscle tone and confidence, among other things.
Vitamin C- The ‘simple’ vitamin C is greatly needed by your adrenal glands. So boosting your supply of this vitamin helps your adrenal glands make more hormones. Food sources include fresh broccoli (not so much week old broccoli), peppers and lemons. As a supplement, look for alma powder or a vitamin C with bioflavonoids. It’s also in the Might Maca powder mentioned above. You can take quite a bit; I’d suggest 1,000 - 3,000 mg/day. Check with your doctor if you have any special medical conditions.
Vitex- Vitex, or Chaste Tree Berry, has a special ability to support your brain’s communication with your ovaries. This can really support a strong ovulation and a resulting high progesterone level in the second part of your cycle.
Foods:
Avoid processed foods, gluten, dairy, sugar, caffeine and alcohol. According to Dr. Tom O’Bryan, author of the Autoimmune Fix, gluten, sugar and dairy are the three biggest triggers of autoimmunity and inflammation. Learn more in my podcast interview of Dr. Tom.
Fill your day with thing like hot lemon water and smoothies in the morning (I like to pair my smoothie with bacon or sausage), generous salad with nuts and beans at lunch, and fish or meat and veggies in a fat-rich sauce at dinner.
If you have low cortisol, you probably also have low blood sugar and will need a couple healthy snacks between meals. Avoid ‘grazing,’ and don’t snack if you don’t need to, but if you tend to crash dramatically without food, then eat more often.
Remember that you don’t have to avoid natural fats to be skinny, you just have to avoid processed carbs!
Healing:
As we learned earlier a leaky gut (increased intestinal permeability), can increase your odds of autoimmune diseases. It can also decrease your odds of get nutrition out of your foods. So your digestive system is important to heal and maintain. Do this by eating a wide variety of plant fibers- aim for twenty different types a week- to feed your friendly gut flora.
If your digestion is weak, cooked food with just a side of raw salad is best for you. Eat in a calm environment and chew your food well. I recommend a high-quality probiotic, and it may require a higher dose while you heal. You can check out the probiotic we love, MegaSpore Biotic, at our Programs and Products page.
You’ll also need to rest (you read that right). Remember earlier how we said that running around without time to rest and reflect can lead to poor food choices? Beyond poor food choices, it can lead to poor life choices! So take some time each day to let your mind unwind. You can read a book, journal, meditate, nap…whatever you like. It’s great to occasionally take a retreat in a natural setting too. Make sure to get a good night’s sleep each night, as critical healing and rebuilding happens nightly.
For cycling women, we offer a Perfect Periods self-study course to help you identify and treat your root causes of low progesterone! Check it out here.
If you’re not yet subscribed to our newsletter, we’d love to have you! You can do so here, and you’ll receive our Hidden Hormone Stressors Quiz, our video “Is My Cycle Normal?’ and our Ten Ways to Destress ebook.
Lastly, feel free to share this article or leave a comment below. Thanks!
Bridgit Danner, LAc, FDNP
A Better Approach to Perimenopause
This is a guest blog article from our friend Dr. Anna Cabeca, MD, OB/GYN. Learn more about Anna and her resources at the close of the article.
HORMONES IN BALANCE ARE GOOD, HORMONE IMBALANCE IS BAD.
What do I mean by that? In healthy menstruating females, hormones cycle on a monthly basis. Our first day of our period is cycle day one, progesterone and estrogen is at their lowest; this is the follicular phase. At around cycle day 12 - 14, ovulation occurs and our progesterone levels increase awaiting a pregnancy, this is the luteal phase of the menstrual cycle, if pregnancy does not occur, progesterone drops and our period occurs again.
Commonly, in our thirties, our progesterone levels start to drop, more than our estrogen levels, creating something called estrogen dominance. This gives us irregular menstrual cycles, possibly heavier bleeding, increased pain with the menses and PMS symptoms such as breast tenderness, irritability, bloating, etc.
We may also begin to lose our sex drive and vaginal lubrication. Our skin may become itchy, noticeably more wrinkled - sometimes this seems to appear overnight - welcome to hormone imbalance!
What can you do about hormone imbalances?
The answer is not just one thing. I always recommend a balanced head to toe approach. My head to toe approach encourages every woman to take control of her health! So, where should the focus be for women at this time?
Focus on the spiritual: What is the mental atmosphere that you find yourself in and what can you do to gain some perceived control of it?
Environment: What are your personal and work environments; and what could be interfering with your ability to achieve happiness? How much nature are you experiencing? Are you getting enough sunlight? When was the last time you walked outside barefoot?
Nutrition: Your body is your temple and what should you be ingesting to nurture it? Is the food you are eating promoting ketosis or fat-burning? Is it alkalinizing? These two principles are key.
Digestion: No matter how well you eat, you have to ensure that you have appropriate digestion - that means adequate acid and digestive enzymes in your stomach and healthy bacterial flora in your intestines to absorb the nutrients. A surprising number of women have poor digestion.
Detoxification: Since the 1950's, corporations have introduced greater than 500,000 chemicals into our environment. Additionally, no matter how we get our hormones, whether it is from what our body naturally produces or from the xeno-estrogens from the environment from pesticides, herbicides, food we eat, air we breathe, etc.; how our body gets rid of it is even more important. All my patients are introduced to my nutrient and protein base detoxification program that includes a modified elimination diet to remove foods, etc., that are likely to produce allergies.
Hormonal balancing: We need to consider the hypothalamic, pituitary, adrenal, and gonadal axis, i.e. the entire hormone web. Additionally, each woman is hormonally unique and part of achieving your optimal health is in understanding this and achieving your own hormonal balance.
Structure and function: Physical strength and exercise are the final and very important aspects to achieving optimal health.
So, when I approach a woman who has symptoms of hormone imbalance, and this is my area of expertise for the last 20 years, we need to incorporate all of the above aspects into a balanced treatment program. For hormone balancing, I consider the major hormones such as adrenaline, cortisol and thyroid, and the hormones estrogen, progesterone, testosterone, and DHEA.
Based on a given individual, I may recommend bio-identical hormone therapy for things such as for treating hot flashes, helping with bones, brain, and heart, improving our sex lives, skin, and energy, and for maintaining our optimal body weight.
My approach has always been to prescribe the lowest doses in the most balanced fashion, based on a given woman’s specific medical history and symptoms, along with test results such as saliva and serum hormone testing. Adding hormones may help, but there are a couple key physiologic lifestyle tips that we must incorporate for optimum success and optimum menopausal experience.
Let me give an example:
Zoe is 43 years old and her periods had gradually becoming more frequent; she complained of more irritability prior to her periods and absolutely no sex drive. And even worse than this – she just felt out of sync. She said that she used to organize all 4 children’s schedules and keep her bills organized, and she volunteered a lot at the school; yet she suddenly felt that she couldn’t even organize her car pool. She had 'lost her edge'.
I took an extensive history, covering all 7 topics above, and did serum, saliva and urinary testing to evaluate hormones and detoxification. She was definitely progesterone deficient, estrogen dominant and also was fatty acid deficient, i.e. she needed more healthy fats, especially omega 3's in her diet. I prescribed a bio-identical progesterone cream and a testosterone cream and in 3 weeks she returned stating she was "feeling better than she had in years!" She had "gotten her edge back". She was also sleeping better, her sex drive returned and her focus and stamina returned. I had also recommended a balanced quality multivitamin, omega 3's, calcium, and a few other nutrients based on nutrient testing such as Co Q 10, Alpha lipoic acid, and carnitine to improve her energy and weight as well.
Her periods became regular, in fact, she stated she couldn't even tell when her periods were coming - the PMS was entirely gone and her relationship with her husband became more satisfying and intimate again.
Dr. Anna Cabeca OB/GYN
It is hard for women, especially because we have so many different roles and obligations, to take the time for ourselves that we need in order to feel our best and perform our best for all those that we love around us.
I encourage each and every one of you to take that time…to remember to try and do as much naturally as you can towards the 7 areas above so that you can achieve your optimal health.
And if you are still struggling with haywire hormones, join me in learning more about the above principles. Take my Menopause Report Card quiz here!
The Four Pillars of Happy Perimenopause with Maria Claps
Before you jump into hormone replacement, or get hooked on mood-altering medications during your perimenopausal years, you need to hear out Maria Claps!
Maria is a health coach and functional medicine practitioner who entered full menopause before 50. But before that, she had a rough ride in perimenopause. After not sleeping for three full days, she broke down and saw a holistic medical doctor. Though she got some relief, she didn't get the careful testing and holistic approach she would have liked.
She went on to become an expert on perimenopause, and now sees, primarily, women ages 45-50 who are complaining of fatigue, low libido, weight gain and low mood.
She developed her approach to hormone health, which she calls the 4 pillars. These include liver care, adrenal support, blood sugar balancing, and hormone testing.
We talk especially about a test we both like, called the Dried Urine Test of Comprehensive Hormones. This test can save you a lot of grief!
Listen in, and learn about Maria's approach.
For more on Maria, see:
Her program "Balance Your Hormones, Love Your Life" which starts May 2, 2016
Or pick up her free perimenopause guide: http://nourishandflourishhealth.com/
Have you joined our online summit yet? It's free, and preview event start 3/30/16! Sign up at Hormones: A Women's Wellness Summit.
See Maria's demonstration on homemade kombucha below:
Is it PMS or Perimenopause?
Cycle Changes After 35 with Andrea Thorpe, MS, LAc, FABORM
If you are experiencing new hormonal symptoms as you age, check out this episode.
Our guest Andrea Thorpe, of Lotus Center of Integrative Medicine in Los Angeles, is an acupuncturist, a functional medicine practitioner, and PhD candidate in Chinese Medicine. She specializes in treating women's health and infertility in her practice, and is often treating women who are 35 and up and stuggling with their hormones.